
 |
|
#166
|
||||
|
||||
|
Re: Sexual Health News
Quote:

|
|
#167
|
||||
|
||||
|
Re: Sexual Health News
What to know about RPR testing for syphilis
https://www.medicalnewstoday.com/articles/322204.php The rapid plasma reagin test is a simple blood test that doctors use to screen for syphilis. The test checks the blood for a current syphilis infection. The rapid plasma reagin (RPR) test looks for specific antibodies that will be present in the blood if a person's immune system is currently fighting off the syphilis virus. If the test identifies an active syphilis infection, a second test will be required to confirm the diagnosis. Once confirmed, a doctor can then start treatment and help prevent further complications or the disease spreading to others. When is the RPR test used? A doctor will likely order an RPR test if a person presents signs and symptoms of syphilis, such as a rash or sores, especially if they have recently had a new sexual partner. A doctor may use an RPR test: To check for an active syphilis infection. To check the progress of a person's condition after they have received treatment. If the treatment is effective, the RPR test will show a decreased number of antibodies in the blood. In routine checkups of sexual health in people who are sexually active. During pregnancy to make sure there are no active infections, as syphilis can affect a growing fetus. Procedure The RPR test follows the same procedure as any other simple blood test. The procedure may take place in a lab or a doctor's office. A person does not typically need to prepare in advance for an RPR test and will not need to fast beforehand. But, always follow the doctor's advice on what to do before, during, and after a medical test. A doctor or technician will tie a rubber tube around the person's upper arm. This will help the blood pool in the vein, making it easier for the technician or doctor to find the vein. Once they find a suitable vein, they will swab the area with antiseptic and use a small needle to collect a small sample of blood. The person may feel a slight pinch. When the technician removes the needle, they will hold some pressure on the site for a few seconds then apply an adhesive bandage to the arm. They then send the blood sample to a lab for testing. Ask the doctor about how long the results will take, as the time frames vary between labs. Interpreting RPR results and accuracy A normal test result typically reveals that the blood does not contain any antibodies that are reactive to syphilis. However, some factors can contribute to syphilis not appearing on the test, which can make the results less accurate. In the early stages of a syphilis infection, the body may not have produced antibodies yet, or not enough antibodies to show up on the test. It can take several months before the antibodies build up. It is also possible that the RPR test fails to detect syphilis after someone has recently received treatment because of the reduced number of antibodies in the blood. It is best to do the RPR test in the middle stages of a syphilis infection — after the body has built up an antibody defense, but before any treatment takes place. Even if the RPR test gives a negative result, a doctor may repeat the test after a few weeks. Other infections can influence the results of an RPR test if they cause the body to produce similar antibodies to syphilis. Some potential infections that could cause a false positive include: malaria lupus Lyme disease HIV some kinds of pneumonia When a person's test results come back as positive, meaning they may have syphilis, their doctor will likely run further tests. These tests, which may include a fluorescent treponemal antibody-absorption (FTA-ABS) test, look specifically for the presence of the antibodies used to fight syphilis. RPR and pregnancy Many states require people to take an RPR test during the early stages of pregnancy. Syphilis represents a significant risk to the fetus, so early detection and treatment can help prevent pregnancy loss due to syphilis infection. In states that do not require the test, a doctor may still recommend that pregnant people take the test, particularly if the doctor suspects that the individual is at a higher risk for contracting syphilis. If the test result is positive, the individual will receive treatment and periodic testing to ensure the infection is under control. Outlook The RPR test is only an initial screening for syphilis. Because there are some problems with its interpretation, further testing is often needed to confirm a syphilis diagnosis. If a person tests positive, they may require an additional test to confirm the presence of syphilis. If a person tests negative, their doctor may request that they repeat the test in a few weeks, especially if they suspect syphilis is present or if a person is considered high risk. Syphilis is a treatable condition and, with treatment, a person can typically expect to make a full recovery. However, if syphilis is left untreated, people may experience severe complications. It is essential to talk to a doctor about the RPR test when experiencing symptoms of syphilis infection. |
|
#168
|
||||
|
||||
|
Re: Sexual Health News
The clitoris: What is there to know about this mystery organ?
https://www.medicalnewstoday.com/articles/322235.php That most elusive part of the female anatomy: the clitoris. What is it, where is it located, and what does it do? How did it develop, and why don't we hear much about it? We answer all these questions and more in this Spotlight. The clitoris has long been misrepresented and misunderstood, and even now, it still holds some riddles that science is yet to solve. All female mammals — and some female birds and reptiles — have a clitoris (or two, as is the case with snakes). However, it is not clear if or how many of them also orgasm thanks to this organ. In humans, the clitoris has been firmly tied to sexual pleasure, though whether it plays any other role is still a matter for debate. Despite approximately half the world's population being born with a clitoris, this sexual organ is not talked about very much, and, until very recently, even the information that we might have found about it in textbooks was incorrect or misleading. So, what is there to know about this elusive organ, and why are we still struggling to understand it? Read on to find out. 1. More than just a 'little hill' The nature of the clitoris can be found in the name itself; "clitoris" comes from the Ancient Greek word "kleitoris," meaning "little hill," and which itself may also be related to the word "kleis," meaning "key." Although this organ may be the key that unlocks female sexual pleasure, it is not just a "little hill," as it has long been believed. In fact, the little hill (protected by a cloak of skin, or the "clitoral hood," which is found over the urethral opening) is just the tip of the much larger organ that is the clitoris. That tip, called the clitoral gland, is the most readily visible part of this genital organ. Yet the entire organ extends much farther than that, and this notion was initially brought to public attention only a few years ago by researcher Dr. Helen O'Connell. "The vaginal wall is, in fact, the clitoris. If you lift the skin off the vagina on the side walls, you get the bulbs of the clitoris — triangular, crescental masses of erectile tissue," Dr. O'Connell explained in an interview with the BBC in 2006. The clitoris has three major components: the glans clitoris, which is the only visible part of the organ, accounting for "a fifth or less" of the entire structure the two crura, which extend, like brackets, down from the glans clitoris and deep into the tissue of the vulva, on either side the two bulbs of the vestibule, which extend either side of the vaginal orifice (not all researchers agree that the vestibular bulbs have a relation to the clitoris, however; researchers Vincenzo and Giulia Puppo, for instance, argue that the clitoris consists "of the glans, body, and crura" only) In its entirety, the clitoris may reach as many as 7 centimeters in length, if not longer, and the glans makes up about 4–7 millimeters of the whole. The glans is also the part that is richest in free nerve endings, thus providing the most sensation. 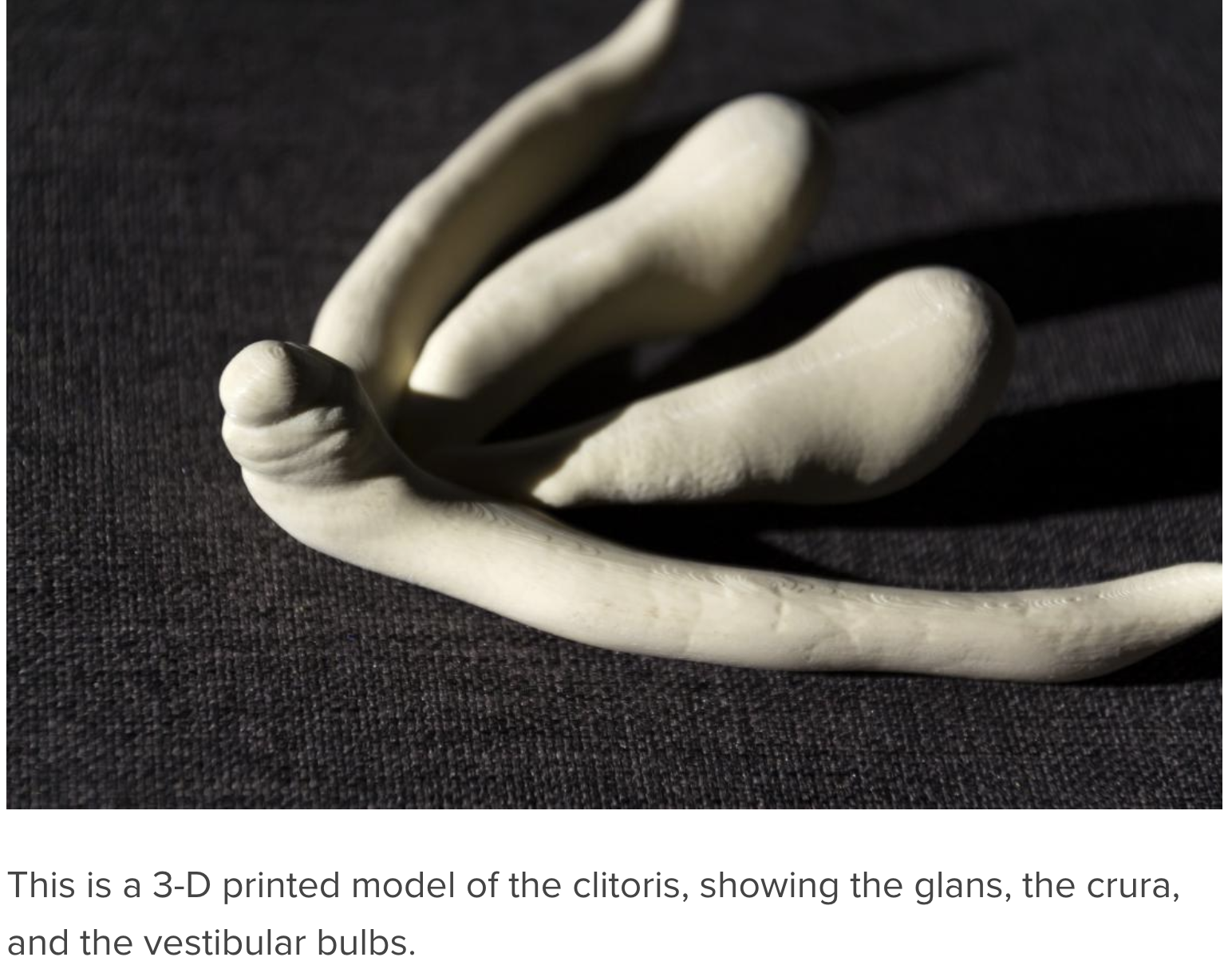 2. 'Grand Central Station of erotic sensation' Due to its high level of sensitivity, the clitoris is usually the main player when it comes to the female orgasm. Popular culture and pornographic material often tend to depict the female orgasm as something usually achievable solely through penetration, but science tells a different story altogether. Most women, researchers have found, will only achieve orgasm when the clitoris — or, more specifically, the glans clitoris — is also stimulated. Sex educator and researcher Emily Nagoski calls the female genital organ the "Grand Central Station of erotic sensation" in her book Come As You Are. In fact, recent studies suggest that women who experience the less common, and sometimes more controversial types of orgasm — vaginal orgasm due to penetration, or vaginal orgasm through G spot stimulation — may actually have clitoral stimulation to thank. 3. A female penis? The clitoris has also sometimes been seen as a female penis, largely due to a phenomenon that we may refer to as "biological homology," which refers to the fact that all fetuses are born, as Emily Nagoski puts it, with "all the same part, organized in different ways." This is also why men — who, unlike women, will not need, or be able, to express milk and breast-feed babies — have nipples. They still develop nipples, however, because they — like pretty much all body parts — are preprogrammed in the earliest stages of embryonic development. In other words, men and women actually mirror each other physiologically to a very great extent. And this is how the clitoris develops; it and the penis are homologues. Nagoski explains how this happens during very early development in the womb. "About 6 weeks after the fertilized egg implants in the uterus, there is a wash of masculinizing hormones," she writes. Quote:
While the penis and the clitoris are homologous, however, the penis plays several roles — erotic, reproductive, and excretive — while the clitoris performs only one job: that of creating erotic sensation, which may lead to orgasm. Why might that be? According to Nagoski, the female orgasm is a "byproduct" of biological homology, and so it should be celebrated as a fantastic bonus. "Male ejaculation, with its close tie to orgasm, is crucial to reproduction," she explains. "As a result, orgasm is embedded on female sexual hardware, too." But some researchers believe that the female orgasm may not always have been "a bonus." Instead, they think that, similarly to male orgasm — which coincides with the release of semen — female orgasm may have stimulated the release of ovules. For instance, the authors of an article that was published in 2016 in the journal JEZ-B Molecular and Developmental Evolution found that immediately after orgasming, women experience a hormonal surge that, in the modern human, has the effect of improving the mood. But the substances thus released in the body, the scientists say, are not unlike those released in the bodies of other female mammals such as rats during intercourse, stimulating the release of eggs that can be fertilized. In humans, ovulation is a spontaneous event, independent from intercourse. But the authors of the aforementioned study hypothesize that, at some point in our evolutionary past, we may well have functioned like other mammals, and female orgasm may have stimulated the release of ovules. Now, orgasm has persisted as a pleasurable evolutionary legacy, without the reproductive association. 5. Why is the clitoris so taboo? But why has it taken so long for scientists to start taking more of an interest in the clitoris, and why is it that someone only took the initiative to scan the clitoris and produce an accurate representation of it in 2009? In an article published in the journal Sex Roles in 2000, researchers Shirley Mattel Ogletree and Harvey J. Ginsburg write that the clitoris had been shrouded in secrecy. Nobody liked to talk about it, and the problem, the investigators suggested, started in the home. They write, "[B]ecause the clitoris's only function is for sexual pleasure, parents have no [...] reason to discuss the clitoris." More shockingly, though, they found, "Even 'experts' providing advice to parents have used terms other than clitoris" when discussing the importance of female genitalia. In a culture that has focused on the importance of reproduction to the detriment of enjoyment, the clitoris has lain forgotten, and the public and medical professionals alike have felt embarrassed to discuss and pay closer attention to it. Yet the lack of a conversation about female genitalia and female pleasure may affect the way in which women understand their sexual health, and it may even impact their sex lives. "Reclaiming the clitoris may help women actively discover their own sexual pleasure and be more independent in the sexual choices that they make," conclude Ogletree and Ginsburg. We hope that this Spotlight can further the conversation about the clitoris, and that it has provided you with further insight into the wonders of female sexuality. |
|
#169
|
||||
|
||||
|
Re: Sexual Health News
Common infections during pregnancy
https://www.medicalnewstoday.com/articles/322210.php During pregnancy, people may worry more about contracting infections and how they might affect the developing baby. Vaginal infections, including yeast infections, are common during pregnancy and are usually not a cause for concern. Uterine infections may produce more complications, however. This article looks at common infections during pregnancy, how they might affect the baby, and how to prevent them from developing. Vaginal infections during pregnancy Someone who is pregnant might be more vulnerable to certain infections and may develop more severe complications if the infections are left untreated. Anyone who has even a minor infection during pregnancy should talk to a doctor or midwife. Typical vaginal infections during pregnancy include: Vaginal yeast infections Vaginal yeast infections are caused by a fungus called Candida. These infections tend to occur during pregnancy because of changes in the immune system, increased production of glycogen, and higher estrogen levels. According to a 2015 report, about 20 percent of all women have Candida, which rises to 30 percent during pregnancy. It appears to be more common during the second and third trimesters. The most common symptoms of a vaginal yeast infection include: itchiness around the vagina or vulva a thick, white, cottage cheese-like vaginal discharge an odor of bread or beer coming from the vagina pain or burning in or around the vagina pain or burning during sexual intercourse People can use prescription or over-the-counter medications to treat a vaginal yeast infection. However, anyone who is pregnant should not use these drugs without first talking to a doctor or midwife. It is essential to get a diagnosis before beginning treatment as other infections, such as bacterial vaginosis and chlamydia, can be confused with yeast infections. Bacterial vaginosis Bacterial vaginosis (BV) is an easily treated bacterial infection in the vagina. Symptoms include: itching, burning, or pain in the vagina or vulva a fishy odor coming from the vagina a bad smell that gets worse after sexual intercourse a large amount of thin, grey colored discharge If BV is left untreated during pregnancy, it might cause preterm labor, premature birth, and lower birth weight babies. Group B Streptococcus (GBS) Group B streptococcus (GBS) is a group of bacteria that come and go in the body but often frequent the vagina and rectum. They do not typically cause symptoms or even an infection. However, women who have GBS in their bodies when they give birth may pass it to their babies. Mothers who have GBS will pass it on to their babies in 1 to 2 percent of cases. Although uncommon, GBS in a newborn can be fatal. Testing late in pregnancy can detect GBS, and is a standard part of most prenatal care. Treatment with antibiotics through a needle in a vein (IV antibiotics) can significantly reduce the risk of a GBS infection passing to the baby. Uterine infections during pregnancy An infection in the uterus can be dangerous for a variety of reasons. The infection may affect the placenta, harm the developing baby, cause premature labor, or lead to birth abnormalities. Uterine infections can also make labor more dangerous and difficult. Some individuals experience organ failure and other life-threatening complications. Uterine infections often develop when bacteria from the vagina travels to the uterus, so an untreated vaginal infection is a risk factor for uterine infections. A person is more susceptible to uterine infections if their membranes rupture during an extended labor. Treatment includes antibiotics and may require hospitalization. If a fever develops during labor, a doctor or midwife will monitor the fetus. If the symptoms are severe, the doctor may recommend a cesarean delivery. Other infections during pregnancy Pregnancy causes many changes in the body, making people more susceptible to complications from many infections. For example, hormone-related skin changes during pregnancy can cause conditions such as eczema or severely dry skin. If the skin cracks open and bleeds, a serious skin infection, such as cellulitis, can develop. A rare skin disorder called Sweet's syndrome is also more common during pregnancy than at other times. Some other infections that may be more serious during pregnancy include: the flu hepatitis E, which is a typically mild viral form of hepatitis herpes, including herpes simplex virus (HSV) and varicella zoster virus (VZV) Listeria, which can cause food poisoning measles HIV The increased risk of these infections during pregnancy is not well understood but may be due to hormone and other changes that alter the number of blood cells in the body. For example, late in pregnancy, T cells that help fight infection decrease in number. Pregnancy also causes increased blood circulation and demands on the heart. These demands can also worsen complications. For example, if a pregnant person develops pneumonia from the flu, they may have more difficulty breathing because of the increased demands the fetus places on the heart and lungs. Some medications that can effectively treat common infections may be less safe during pregnancy. So it is essential that pregnant people who have an infection talk to their doctor or midwife to weigh up the benefits and risks of various treatment options. How do maternal infections affect the baby? Numerous infections can affect the developing baby. However, it is difficult for doctors to tell whether and to what extent a fetus will be affected. Infections can affect a developing baby in one of three ways: They may harm the mother, making her body less able to nurture the baby or requiring the use of drugs that may harm a fetus. They can directly harm the baby by causing changes that lead to birth abnormalities. They can trigger premature labor or a miscarriage. According to the National Institutes of Health (NIH), infections that are known to harm the developing baby include, but are not exclusive to: bacterial vaginosis, which might cause preterm labor contagious diseases, such as hepatitis, syphilis, herpes, and HIV, which can infect the fetus chlamydia, which can cause eye infections and pneumonia gonorrhea, which can contaminate the amniotic fluid, cause preterm labor, and lead to eye infections and possible blindness fifth disease, which can trigger a miscarriage or cause fetal anemia group B streptococcus, which can cause severe complications in newborns, and in rare cases can be fatal toxoplasmosis, which can cause birth abnormalities and intellectual disabilities Listeria, which can cause miscarriage, stillbirth, and birth abnormalities cytomegalovirus, which is often harmless but can also cause birth abnormalities and intellectual disabilities Zika, which is usually mild, can cause pregnancy loss or birth abnormalities in an infant Zika infection, which is a disease carried by mosquitoes, may cause birth abnormalities and increase the risk for stillbirths and miscarriages in those who have the virus. However, it is unclear why some fetuses are affected, and others are not. Other infections may also harm a developing baby, depending on the overall health of the pregnant person, when the infection developed, and whether the person has received treatment. Preventing infections The Centers for Disease Control and Prevention (CDC) provide some strategies to reduce the risk of developing an infection during pregnancy, including: avoiding travel to areas where Zika is prevalent, and using bug spray to prevent mosquito bites using a condom and asking a partner to be tested for sexually transmitted infections (STIs) washing hands carefully and diligently avoiding people who have contagious infections getting a flu shot avoiding unpasteurized foods asking someone else to change the cat litter testing for STDs and group B strep Outlook Most people who experience an infection during pregnancy will not experience complications. Prompt treatment increases the likelihood of a healthy birth. Anyone who experiences any unusual symptoms during their pregnancy should talk to their doctor or midwife. Prenatal care is also crucial since it can detect certain infections even before they cause symptoms. |
|
#170
|
||||
|
||||
|
Re: Sexual Health News
What do white spots on testicles mean?
https://www.medicalnewstoday.com/articles/322213.php White spots on the testicles can have several different causes, which range from harmless to more serious health conditions. They are usually not a cause for concern, but may still require treatment. The spots can also sometimes be a sign of a sexually transmitted infection (STI). This article discusses the possible causes of white spots on the testicles, how to prevent and treat them, and when to see a doctor. Causes There are several possible causes for white spots on the testicles, and each will require a different treatment approach: Whiteheads Whiteheads are a form of acne that occurs when the pores under the skin become clogged with oil, dead skin, or other debris. These blockages can cause inflammation and the development of a rounded lump. Each lump may have the fleshy-white coloring that characterizes a whitehead. Whiteheads typically develop in areas with a high concentration of pores, such as the face or chest, but they can also develop on the testicles. They generally do not cause other symptoms and pose no serious health risk. Treatment Whiteheads usually resolve without treatment. However, it is possible to treat whiteheads using over-the-counter (OTC) medications such as benzoyl peroxide or salicylic acid. The testicles are a sensitive area, so anyone who experiences skin irritation should cease treatment. Ingrown hairs Ingrown hairs occur when a hair grows back into its follicle below the skin surface. They can occur anywhere on the body where hair grows, including around the testicles. Ingrown hairs cause itchy, sore bumps to develop, which can be uncomfortable. It is also possible for them to become infected, leading to folliculitis. Treatment Most ingrown hairs clear up without treatment. However, using an exfoliant to remove dead skin cells can accelerate the healing process. It is essential to avoid scratching ingrown hairs as this will slow down the healing process and increase the risk of infection. Applying a steroid cream may help to relieve itching. Folliculitis Folliculitis is a condition in which the hair follicle becomes inflamed. It often occurs as a result of infection and can cause the emergence of spots that contain pus. These spots can be itchy and uncomfortable, but they are not harmful. Treatment Most cases of folliculitis are mild and will clear up after a few days without the need for treatment. Refraining from shaving the area and from wearing tight underwear can help. Topical antibacterial or antifungal medications are available OTC and can help to clear the infection more quickly. Genital warts and blisters STIs, such as the human papillomavirus (HPV) and herpes simplex virus (HSV), can cause genital warts and blisters, respectively. Genital warts may appear as white, brown, or flesh-colored bumps that grow on and around the testicles. These warty bumps can be itchy but are usually not painful. The fluid-filled small blisters of HSV can burst and ooze fluid and may be itchy and painful. Treatment Genital warts resulting from HPV may clear up on their own, but more persistent cases might require treatment. To treat HPV, doctors may recommend using a cream that supports the immune system in removing the wart, such as imiquimod cream. In some cases, cryotherapy or surgery may be necessary to remove the wart. The standard treatment for genital blisters resulting from HSV is antiviral medication, which reduces the activity of the virus, but does not kill the virus itself. However, both of these STIs are chronic infections. A person with HPV may find that warts recur, while someone with HSV may have recurring blisters. Fordyce spots Fordyce spots are small, yellow-white bumps. They occur when the sebaceous glands that secrete oil onto the skin become enlarged. These sebaceous glands are separate from hair follicles. Fordyce spots are more common on the lips and inner cheek, but they can also occur on the genitals. They are harmless, and it is not possible to transmit them sexually. Treatment Fordyce spots do not require treatment as they do not cause any other symptoms and are not a health risk. However, it is possible to treat them with creams and surgery if people do want to remove them. Syphilis Syphilis is an STI that can cause white ulcers to develop on the testicles. It occurs as a result of infection with Treponema pallidum, a highly-infectious bacterium. Without treatment, syphilis can have serious health consequences, including paralysis and dementia. Treatment People with syphilis require antibiotic therapy. They must begin the course of treatment as soon as possible, as it is not possible to reverse any permanent damage that the condition causes. Even after successful treatment, a person may contract syphilis again at a later date. Prevention The most effective way to prevent many causes of white spots on the testicles is to avoid unprotected sexual activity. This will lower the chances of contracting an STI, which can cause white spots to develop as a symptom. Other more general tips to reduce the likelihood of white spots developing on the genitals include: avoiding tight underwear washing the testicles regularly spending minimal time in hot climates washing after sports or activities that induce sweating Some causes, such as Fordyce spots, may not be possible to avoid. When to see a doctor If the spots do not disappear within a couple of weeks of using non-prescription treatments, it is best to speak to a doctor. A doctor can determine if the spots are due to a more severe health condition and provide advice on the most appropriate treatment approach. If other symptoms occur with the spots, it is vital to see a doctor immediately. These could include: skin rashes abnormal discharge pain swelling burning sensation when urinating genital pain after sex Outlook There are several possible causes of white spots on the testicles. In many cases, the spots will be harmless, but some people may want treatment to remove them. Anyone with additional symptoms alongside the white spots should see a doctor. |
|
#171
|
||||
|
||||
|
Re: Sexual Health News
A color-coded guide to vaginal discharge
https://www.medicalnewstoday.com/articles/322232.php It is common to wonder whether the color or consistency of vaginal discharge is normal or needs to be checked out. Vaginal discharge can be many colors, and several indicate a healthy body. In this article, we provide a color-coded guide to vaginal discharge. Learn what the colors mean and when to see a doctor. What is vaginal discharge? Vaginal discharge is fluid secreted from tiny glands in the vagina and cervix. This fluid leaks from the vagina each day to remove old cells and debris, keeping the vagina and reproductive tract clean and healthy. The amount of vaginal discharge can vary significantly from person to person. The color, consistency, and amount can also change from day to day, depending on where a person is in their menstrual cycle: Days 1–5. At the beginning of the cycle, discharge is usually red or bloody, as the body sheds the uterine lining. Days 6–14. Following a period, a person may notice less vaginal discharge than usual. As the egg starts to develop and mature, the cervical mucus will become cloudy and white or yellow. It may feel sticky. Days 14–25. A few days before ovulation, the mucus will be thin and slippery, similar to the consistency of egg whites. After ovulation, the mucus will go back to being cloudy, white or yellow, and possibly sticky or tacky. Days 25–28. The cervical mucus will lighten, and a person will see less of it, before getting another period.  The shade of red can vary from bright to a dark rust color. Red discharge is most commonly the result of bleeding during a period. Menstrual bleeding happens, on average, around every 28 days, though the normal range between 21 and 35 days. A period typically lasts for 3–5 days. Anyone who experiences bleeding between menstrual periods should see a doctor. Though there are many benign causes of intermenstrual bleeding, it can sometimes signal a serious condition. Anyone who has gone through menopause and not had a period for at least 1 year should see a doctor if they experience vaginal bleeding. It can sometimes be a sign of endometrial cancer. 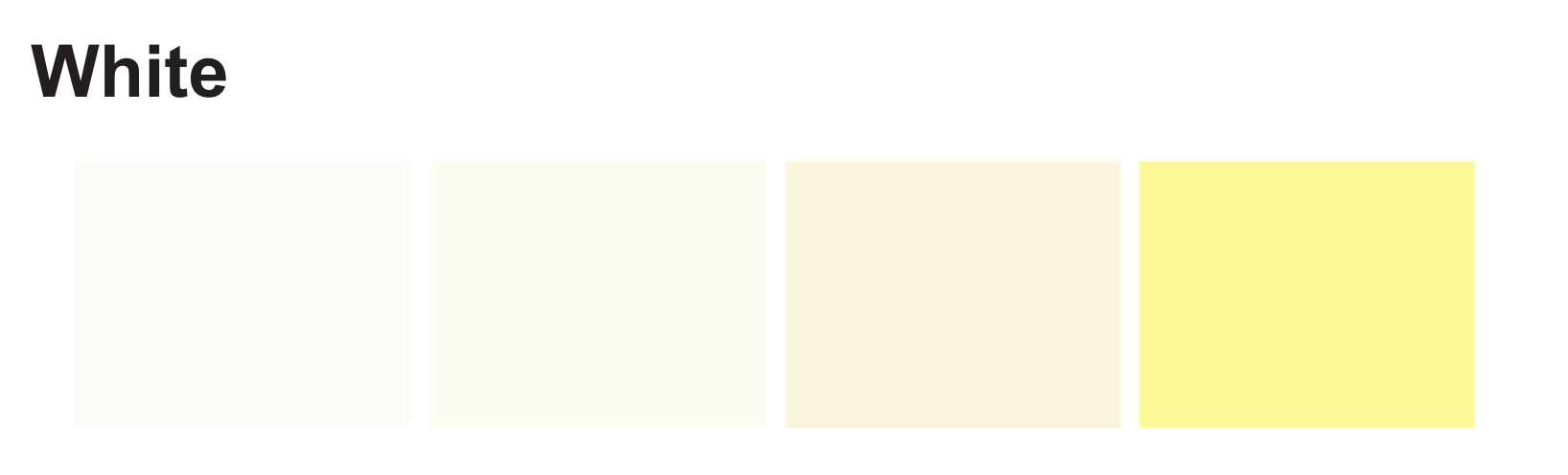 The shade of white can extend to include cream or light yellow. If a person has no other symptoms, white discharge is most likely a sign of healthy lubrication. However, if the white discharge has a consistency like cottage cheese or is accompanied by a strong odor, it can indicate an infection. An individual should see a doctor. White, thick, strong-smelling discharge is usually associated with a yeast infection, which can also cause itching or irritation. Yellow-green  If the discharge has a very slight yellow hue, it may not indicate a problem. This is especially likely if the hue only coincides with a change in diet or dietary supplements. Discharge that is a darker shade of yellow, yellowish-green, or green usually signals a bacterial or sexually transmitted infection. See a doctor promptly if vaginal discharge is thick or clumpy, or it has a foul odor. Pink  Discharge can be light or a much deeper pink. It usually contains a little bit of blood. Pink discharge most commonly occurs with spotting before a period. However, it can also be a sign of implantation bleeding in early pregnancy. Some people experience a little bit of spotting after ovulation, which can also cause pink discharge. Discharge can be pink after sexual intercourse if the sex has caused small tears or irritation in the vagina or cervix. Clear Most ordinary vaginal discharge is clear or whitish. It may be slippery or have the consistency of egg whites. A person is likely to experience more clear, slippery discharge just before ovulation, during sexual arousal, and during pregnancy. Gray  Gray vaginal discharge is not healthy, and it can be a symptom of a common bacterial infection called bacterial vaginosis (BV). BV usually causes other vaginal symptoms as well, including: itching irritation a strong odor redness around the vulva or vaginal opening Anyone with gray discharge should promptly see a doctor. Following diagnosis, the doctor will usually prescribe antibiotics to treat the BV. When to see the doctor See a doctor if vaginal discharge has an unusual smell or appearance. A person should also seek medical care if they experience vaginal symptoms such as: itching pain or discomfort discharge that is frothy or like cottage cheese bleeding between periods or after menopause spotting after sex regularly grey, green, or yellow discharge a strong odor a burning sensation during urination The doctor will perform a pelvic exam. They may also need to take a sample of discharge for testing. Outlook Below is a summary of causes for each color of vaginal discharge: 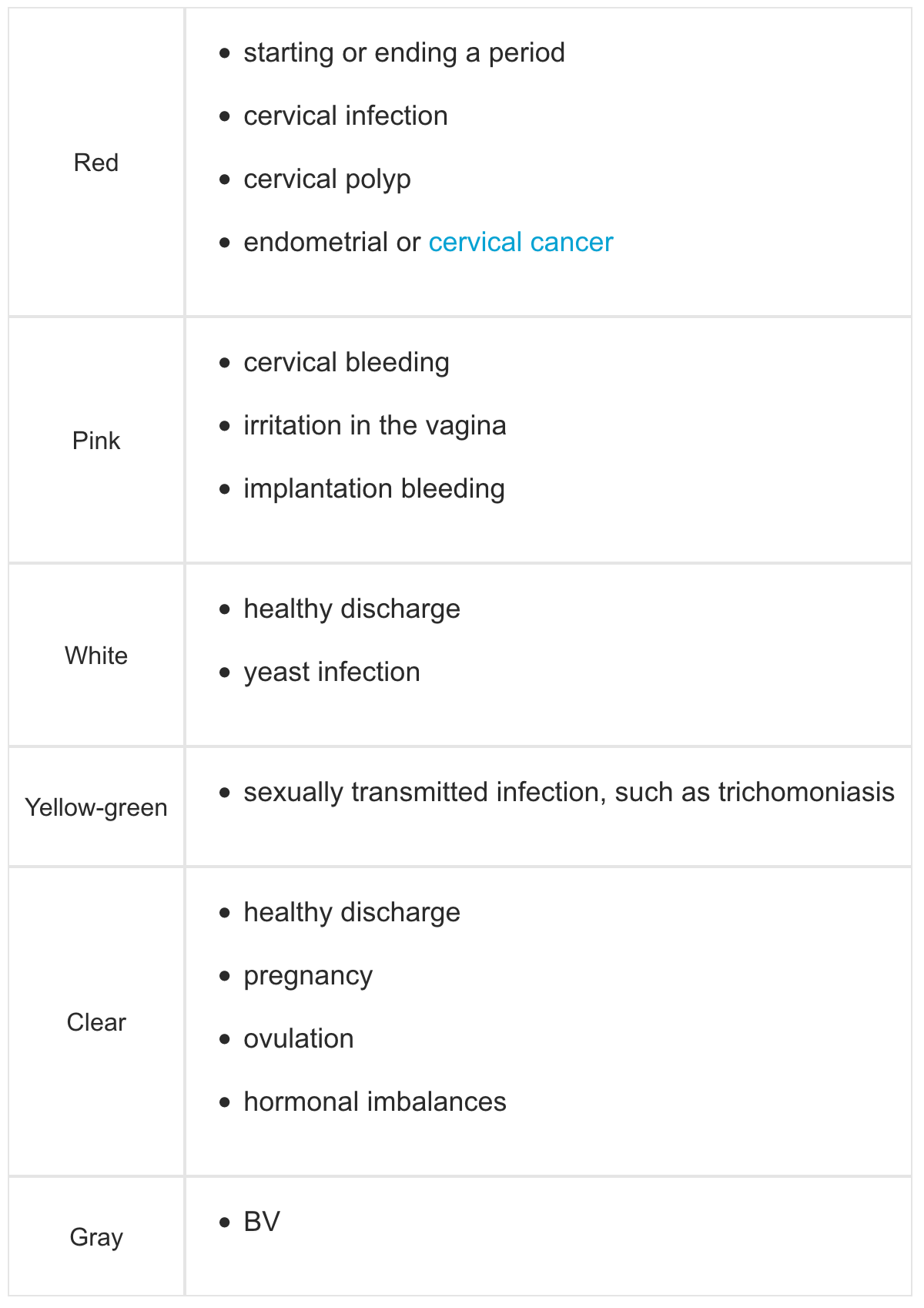 In most people, infections or hormonal imbalances are responsible for unusual changes in vaginal discharge. Medication may be necessary. A person should see a doctor if they notice irregular changes in vaginal discharge or other symptoms that might indicate a reproductive health issue. |
|
#172
|
||||
|
||||
|
Re: Sexual Health News
What to know about anal herpes
https://www.medicalnewstoday.com/articles/322294.php Herpes is a viral infection that can cause blisters and sores around the mouth, genitals, or anus. Herpes that affects the anus is called anal herpes. Herpes does not always cause symptoms. When it does, people with anal herpes may notice blisters or sores in or around their anus. Because the symptoms are similar, anal herpes may be confused with hemorrhoids or syphilis. In this article, we give an overview of anal herpes, including how to identify and diagnose the condition, treatment for it, and how to reduce the risk of infection. What is anal herpes? The herpes simplex virus causes all types of herpes. It is a contagious virus, meaning that people can catch it from physical contact with each other. Sexual contact is often how genital herpes and anal herpes are transmitted. Because of this, they are considered sexually transmitted infections or STIs. There are two kinds of herpes virus: herpes simplex virus type 1, or HSV-1, which primarily affects the mouth herpes simplex virus type 2, or HSV-2, which mostly affects the genitals and anus HSV-2 causes most cases of anal herpes in humans and sexual contact with an infected individual is how the virus is transmitted. The World Health Organization estimates that 417 million people, or 11 percent of those aged 15–49 years of age worldwide, have the HSV-2 infection. Symptoms Many people do not experience symptoms immediately, and the infection can go undetected for years. Even if people have no symptoms, they can transmit the infection to others. Common symptoms of anal herpes include: persistent pain or itching around the anus red bumps or colorless, painful blisters blisters, sores, or ulcers around the anus change in bowel habits Diagnosis The symptoms of anal herpes are similar to the symptoms of several other conditions, including hemorrhoids and syphilis. A doctor may be able to identify the condition by sight or physical examination. Doctors may recommend a blood test to look for the herpes virus. Otherwise, they may take a swab of the affected area and use the sample to run a DNA test called nucleic acid amplification testing, or NAAT. These newer tests are fast, accurate, and can tell if a person has an HSV-1 or HSV-2 infection. Treatment Since anal herpes is a viral infection, treatment is usually with antiviral medications. These types of drugs fight off the virus activity in the system and help reduce or control symptoms. Antiviral medicines also reduce the duration of the infection and the risk of the virus being passing on to a sexual partner. Doctors should treat people as soon as possible since early treatment decreases the risk of transmission to others. Examples of antiviral medicines to treat anal herpes include Famvir, Valtrex, and Zovirax. Risk factors Intimate sexual contact with an infected person is how anal herpes spreads. Hence, people can get anal herpes by having vaginal, anal, or oral sex with a person who has the virus. Direct mouth or skin contact allows the virus to be transmitted easily via: herpes sore or scab saliva genital secretions Below is a 3-D model of herpes which is fully interactive. Explore the 3-D model, using your mouse pad or touchscreen, to understand more about herpes.  Prevention Anal herpes is contagious, but not everyone with the herpes virus shows symptoms. This means that people can contract the virus without their knowledge. Ways to reduce the risk of contracting herpes include: using barrier protection, such as condoms, during vaginal, anal, and oral sex getting regular sexual health screenings for STIs making sure that all sexual partners undergo routine sexual health screening If someone's sexual partner has anal herpes, they can lower the risk of transmission by using barrier contraception and avoiding sexual activity when their partner has an outbreak or active infection. People who have had herpes should take any prescribed antiviral medication, as instructed by a doctor, and attend follow-up appointments to make sure they keep the virus under control. Can anal herpes be cured? There is no current cure for HSV-2 infections so the condition may require lifelong management. However, even if people have the herpes virus, it will not always produce symptoms and is not always transmissible. The infection is known to recur in some people under certain conditions that re-activate the virus, such as illness, stress, sunlight, or fatigue. Repeated outbreaks tend to be shorter and less severe than the first outbreak. Although the virus remains in the body for the rest of the person's life, the number of outbreaks may gradually decrease over time. Summary Anal herpes is a type of genital herpes. It is more common today than it was some decades ago. While doctors cannot cure the infection, there are now many antiviral medicines available that reduce symptoms and decrease the risk of transmitting it to others. Awareness is key to reducing the spread of anal herpes, as is practicing sex with condoms and following good personal hygiene. |
|
#173
|
||||
|
||||
|
Re: Sexual Health News
What to know about sex and yeast infections
https://www.medicalnewstoday.com/articles/322483.php Yeast infections occur because of an overgrowth of a type of fungus known as Candida, which lives in the body harmlessly most of the time. It is possible to have sex with a yeast infection, but it can be painful and has other risks. According to the Centers for Disease Control and Prevention (CDC), vaginal yeast infections are the second most common kind of vaginal infections after bacterial infections of the vagina. Symptoms of a vaginal yeast infection can include: vaginal pain or soreness pain during urination itching or burning pain during sex thick, white vaginal discharge Can you have sex if you have a yeast infection? While it is possible for a person with a yeast infection to have sex, most doctors do not recommend having sex until the infection has cleared up. Also, because many of the symptoms are uncomfortable, individuals may choose to refrain from sexual activity while they have a yeast infection to minimize pain and itching. As well as being painful or uncomfortable, a person who has sex while they have a yeast infection may cause the infection to last longer, cause symptoms to return if they have recently cleared up following treatment, and increase their partner's risk of developing a yeast infection as well. Transmission during sex Sexual partners can transmit yeast infections. However, the likelihood of transmission is small. When a woman has sex with another woman, there is some evidence to suggest they can transmit a yeast infection. However, one study found no evidence supporting the transmission of the infection from woman to woman through sex. While yeast infections in men are rare, it is possible for a man to get an infection by having sex with a person who has a vaginal yeast infection. Uncircumcised men are more susceptible to developing a yeast infection. A yeast infection is not a sexually transmitted infection (STI). However, some prevention methods, such as condoms, can help reduce the risk of spreading a yeast infection to a partner. How long should you wait after treatment? Having sex while undergoing treatment for a yeast infection may slow down the healing process. Also, if a person's partner develops a yeast infection, it is possible that the infection will get passed back and forth. A person should generally avoid sexual activity until all the symptoms clear up. Yeast infections usually clear relatively rapidly once a person begins treatment. Many over-the-counter (OTC) treatment options require up to 7 days to clear up the infection. Causes The fungus Candida causes yeast infections. This fungus lives in and on various parts of the human body, including the skin, the mouth, and the vagina. In the vagina, the Lactobacillus bacteria typically keeps Candida numbers in check. If there is a shortage or imbalance of Lactobacillus compared to Candida, a yeast infection may occur. Some common causes of a bacterial imbalance in the vagina include: uncontrolled diabetes immunosuppression, such as having HIV a hormone imbalance stress pregnancy excessive sugar consumption taking antibiotics Most yeast infections are easy to treat. However, if a person experiences multiple, recurring yeast infections, they should speak to a doctor as Candida may not be the underlying cause or OTC remedies may be ineffective. Symptoms Symptoms of a yeast infection include: pain during sex burning sensation during sex or urination itchiness redness a rash swelling of the labia white, clumpy discharge When left untreated, the symptoms will typically get worse. However, some mild yeast infections may get better without treatment. When to see a doctor People can often treat a yeast infection at home using OTC remedies. These treatments usually contain one of the following ingredients: butoconazole (Gynazole) miconazole (Monistat) terconazole (Terazol) When a person develops a yeast infection for the first time, they should see a doctor to ensure they receive the correct diagnosis and treatment. People should also seek medical advice if OTC treatments are not effective. A doctor may recommend alternative treatments, including oral medication. Finally, a person should seek medical attention if they: have four or more yeast infections in a year are pregnant have severe symptoms have a compromised immune system Once the treatment is complete, and the symptoms are gone, a person can return to their regular sex life. |
|
#174
|
||||
|
||||
|
Re: Sexual Health News
What to do about a smelly penis
https://www.medicalnewstoday.com/articles/322562.php In most cases, regularly cleaning the penis keeps odor to a minimum. However, some conditions may cause the penis' odor to change or smell foul. Often, using simple home remedies will reduce penis odor. However, some conditions require medical treatment. In this article, we look at common causes of a smelly penis, as well as how to treat them. Six causes of a smelly penis Causes of a smelly penis can include: Smegma Smegma is an accumulation of dead skin cells and the natural oils that keep the penis moist. If a person does not clean their penis regularly, the smegma can build up, resulting in a thick white substance. This buildup is more common on uncircumcised penises as it forms around the head of the penis. In addition to a bad smell, smegma can: cause redness and irritation prevent the foreskin from easily moving when the penis is erect increase the risk of a bacterial infection Balanitis Balanitis is skin irritation on the tip of the penis. Some of the primary causes of balanitis include: poor hygiene infections skin conditions, such as psoriasis allergic reactions to medications, soaps, or condoms If a person suspects balanitis may be the cause of a bad smell, they should talk to a doctor about possible treatments. Sexually transmitted infection (STI) STIs may cause a smelly penis, in some cases. The two STIs most likely to cause penis odors are chlamydia and gonorrhea. Symptoms of chlamydia include: white, watery discharge from the penis pain while urinating testicle pain Symptoms of gonorrhea include: green, white, or yellow discharge from the penis pain or burning while urinating inflammation in the foreskin Anyone who suspects they may have an STI should seek medical attention and refrain from sexual activity until they have finished treatment. Non-gonococcal urethritis (NGU) NGU is inflammation of the urethra, which is the tube connecting the tip of the penis to the bladder. In most cases, inflammation of the urethra is due to an STI, such as chlamydia. However, in cases of NGU, the cause of the swelling is unknown. Symptoms of NGU may include: cloudy or white discharge from the penis frequent urge to urinate burning or painful urination irritation or soreness near the tip of the penis Yeast infection A yeast infection occurs when too much of the Candida fungus is present on the penis. While vaginal yeast infections are much more common, yeast infections can also affect the penis. In addition to a bad smell, other symptoms of a yeast infection include: burning or itching sensation irritation and redness on the penis a white substance with a cottage cheese consistency unusual moisture on the penis It is essential to seek medical treatment for a yeast infection, as it may lead to further infections and complications. Urinary tract infection (UTI) A UTI occurs when bacteria or a virus gets into the urinary tract. UTIs can cause: a smelly penis pink or cloudy urine frequent urges to urinate burning sensation when urinating Risk factors for developing UTIs include: kidney stones an enlarged prostate sexual activity diabetes a urinary catheter Treating a UTI can help prevent further complications, including kidney problems or the infection spreading beyond the urinary tract. How to clean the penis Practicing proper hygiene can help avoid infections and reduce any odor coming from the penis. It is essential to wash the genitals at least once a day with a gentle cleanser and warm water. After cleaning the penis, a person should make sure the area is completely dry before putting on clothing. In addition to daily washing, a person should consider taking some additional steps to keep the penis odor-free. These steps include: cleaning the penis after engaging in sexual activity wearing loose-fitting, breathable clothing using barrier protection, such as condoms, during sexual activity avoiding sexual activity when either partner has an STI or other infection cleaning under the foreskin if uncircumcised Treatment and home remedies Treating a smelly penis depends largely on what is causing the smell. If a lack of correct hygiene is an issue, a person can gently wash their penis more regularly with warm water. It is best to avoid heavily scented products on the genitals, as they can irritate the skin and increase a person's risk of infections. People should also refrain from using cologne, scented cream, or other perfumes directly on the penis. If a person suspects they have an infection, they should see a doctor for a diagnosis and treatment. Treatment may include antibiotics, antifungal medications, or other medications. When to see a doctor A person should see a doctor if any of the following symptoms accompany a smelly penis: unusual discharge pain or burning during urination increased need to urinate irritation and redness on the outside of the penis Outlook In most cases, a person can treat a smelly penis with simple techniques at home, starting with better hygiene. If other symptoms are present, such as pain, irritation, or discharge, it is best to see a doctor for a proper diagnosis. |
|
#175
|
||||
|
||||
|
Re: Sexual Health News
What causes vaginal cramps?
https://www.medicalnewstoday.com/articles/322584.php Vaginal cramps or spasms may feel like strong, painful muscle contractions. While mild vaginal cramps can be a symptom of menstruation, painful cramps or vaginal cramps that occur outside of menstruation often have an underlying medical cause. This article looks at some of the most common causes of vaginal cramps, as well as treatment options and when to see a doctor. Causes Possible causes of vaginal cramps include the following: Infections Vaginal infections can cause vaginal cramps, sharp pain, inflammation, and discomfort. Common types of vaginal infection include: bacterial vaginosis sexually transmitted infections (STIs), such as trichomonas urinary tract infections (UTIs) yeast infections Infections can also cause fever and unusual discharge, which may be foul-smelling. Menstruation Vaginal cramps are a common symptom of menstruation. They occur as the uterus contracts to shed the uterine lining. Although cramps higher up in the pelvis are more common, it is not unusual to feel cramping in the vagina as well. While doctors would expect some mild cramping during menstruation, severe pelvic pain and bleeding are not typical period symptoms. A doctor can prescribe medications, such as birth control pills, to reduce the incidence of pelvic pain and discomfort resulting from menstruation. Dyspareunia Dyspareunia is the medical term for painful sex. This pain may occur during or immediately after sex. Some people also experience dyspareunia when they use tampons. Dyspareunia typically feels like menstrual cramps with the addition of a deep, burning pain inside the pelvis. Multiple causes of dyspareunia exist, including infections, inflammation, and a history of surgery on the vagina or uterus. Endometriosis Endometriosis is a condition that occurs when cells resembling uterine tissue grow outside the uterus. This tissue contracts and bleeds during menstruation, but it cannot exit the body. This can result in significant pain and cramping. If endometriosis develops in the vagina, it can cause cramping in this area. However, some people with vaginal cramping may be experiencing referred pain. Referred pain means that the tissue is contracting in other areas of the body, but the individual feels the pain in the vagina instead. Pelvic floor disorders Pelvic floor disorders are conditions that cause pain, cramps, and other symptoms in the pelvic floor muscles, which support the bladder, rectum, and uterus. These disorders may occur after a woman has given birth, as delivery can weaken the pelvic floor. In addition to vaginal cramps, pelvic floor disorders can lead to constipation, pain during sex, and difficulty controlling a urine stream. Pelvic inflammatory disease (PID) PID is a condition that occurs when an infection in the pelvic organs causes inflammation in the vaginal tissue. Symptoms can range from mild to severe, and may include: bleeding between periods pain in the lower abdomen pain during sex unusual discharge from the vagina or an odor vaginal cramps People who have STIs, such as gonorrhea or chlamydia, are more likely to experience PID. Uterine fibroids Uterine fibroids are non-cancerous growths that develop in the uterine wall. They are most common in people who are in their 30s and 40s but tend to go away after menopause. Uterine fibroids can cause heavy bleeding, vaginal cramps, pain during sex, and a feeling of fullness or pressure in the lower abdomen. Vulvodynia Vulvodynia is a medical condition in which a person experiences pain in the vulva, the external female genitalia, for 3 months or longer without any known cause. Miscarriage Miscarriage, or pregnancy loss, occurs when a pregnancy ends at or before 20 weeks of gestation. In addition to vaginal cramps, miscarriage can cause spotting or bleeding and pain in the abdomen. Vaginal cramps during pregnancy Vaginal cramps may occur during pregnancy for a variety of reasons. Mild cramps may be due to the implantation of the placenta or to cervical cell changes. The growing uterus can also put pressure on the surrounding pelvic organs, causing some discomfort. Vaginal cramps in the first 20 weeks of pregnancy can also indicate a miscarriage if bleeding accompanies them. Sometimes, vaginal cramps during pregnancy can indicate that the baby's delivery is imminent. If this occurs less than 37 weeks into the pregnancy, it is advisable to call a doctor to ensure that the symptoms do not indicate preterm delivery. Together with contractions, vaginal cramping helps to make changes in the cervix to prepare the body for delivery ahead of the due date. Vaginal cramping shortly before delivery may result in sharp or stabbing pains, which can indicate that the cervix is dilating to prepare for the birth. When to see a doctor While people can expect some mild vaginal cramps during menstruation, other instances of vaginal cramping can indicate underlying but usually treatable health issues. A person should speak to a doctor if they are experiencing any of the following symptoms in addition to vaginal cramps: foul-smelling or unusual discharge a sensation of pelvic fullness and pressure heavy or unexplained bleeding severe pain pain during sex trouble controlling urination or feelings of urinary urgency If a pregnant woman is concerned about vaginal cramps, especially those occurring alongside bleeding, she should speak to a doctor. Takeaway While mild vaginal cramps are often a standard symptom of menstruation, severe or recurrent cramps may have an underlying medical cause. A doctor can provide an accurate diagnosis and recommend treatment options to alleviate pain and reduce the frequency of vaginal cramps. |
|
#176
|
||||
|
||||
|
Re: Sexual Health News
Do erectile dysfunction exercises help?
https://www.medicalnewstoday.com/articles/322600.php Erectile dysfunction occurs when a man cannot get or maintain an erection. It is common in men of all ages. Muscles, especially those important in maintaining an erection, sometimes lose tone and strength. As a result, exercises can help to reverse erectile dysfunction (ED). Causes and risk factors for ED include: obesity cardiovascular disease metabolic syndrome prostate cancer stroke low levels of physical activity smoking alcohol use Doctors may prescribe phosphodiesterase type 5 inhibitors, such as Viagra, for ED. Lifestyle changes, including exercise and weight loss, are also effective in treating ED. Exercise vs. other treatments Treating the cause of ED will have long-lasting results, while medication only provides temporary relief. Also, some people find medication to be ineffective. Sometimes, psychological factors are responsible for ED. In these cases, a person can benefit from forms of talking therapy. What types of exercise can help? Exercises that strengthen the muscles of the pelvic floor can benefit people with ED. The pelvic floor muscles are key in sustaining blood flow to the penis and maintaining erections. The muscles do this by putting pressure on the penile veins. The pressure prevents blood from leaving the area, making an erection possible. Kegel exercises to try Pelvic floor exercises, or Kegels, are the most beneficial for ED. These exercises target the muscles at the bottom of the pelvis, and particularly one called the pubococcygeus. This loops from the pubic bone to the tailbone and supports the pelvic organs. When this muscle weakens, it is unable to prevent blood from flowing out of the erect penis. Performing pelvic floor exercises will strengthen and improve tone in the pubococcygeus. It can take 4–6 weeks before a person notices a difference in erections. 1. Activating pelvic floor muscles This exercise is simple but important. It teaches a person to activate their pelvic floor muscles. Lie down with the knees bent, the feet flat on the floor, and the arms by the sides. Exhale and squeeze the pelvic floor muscles for a count of three. Inhale and release for a count of three. Take time identifying the right group of muscles — those at the bottom of the pelvis. It can be easy to accidentally contract other muscles instead, particularly those of the stomach, buttocks, or legs. 2. Sitting pelvic floor activation Sit with the arms at the sides and the feet flat on the floor, hip-width apart. Using the same technique as above, activate the pelvic floor muscles for a count of three, and release for a count of three. Ensure that the stomach, buttocks, and leg muscles are not contracting. 3. Standing pelvic floor activation Stand straight with the arms by the sides, and the feet hip-width apart. Using the technique above, activate the pelvic floor muscles for a count of three, and release for a count of three. Ensure that the stomach, buttocks, and leg muscles are not contracting. Once a person is comfortable performing Kegel exercises three times a day, it can help to add exercises that involve more movement. Pilates exercises to try These Pilates exercises activate the right group of muscles and challenge a person to maintain pelvic floor strength while moving. 4. Knee fallouts This is a beginners' exercise that involves small movements. Lie down with the knees bent, the feet flat on the floor, and the arms by the sides. Keep the spine in a neutral position, with a small space between the middle of the back and the floor. Exhale, squeeze the pelvic floor muscles, and slowly lower one knee to the floor. Only lower it as far as possible while maintaining activation of the pelvic floor muscles. Keep the pelvis stable. Inhale, release the muscles, and bend the knee again. Repeat on the other side. Start with four or five repetitions on each side and build up to 10. 5. Supine foot raises This exercise builds on knee fallouts and involves small movements. Lie down with the knees bent, the feet flat on the floor, and the arms by the sides. Exhale, engage the pelvic floor muscles, and slowly raise one foot off the floor. Keep the pelvis and the spine still. Inhale, lower the foot back to the ground. Alternate sides. 6. Pelvic curl This exercise is common in Pilates. Lie down with the knees bent, the feet flat on the floor, and the arms by the sides. Keep the spine in a neutral position, with a small space between the middle of the back and the floor. Exhale, and engage the pelvic floor muscles. Tilt the pelvis upward toward the belly button, while pressing the back flat against the floor. Slowly lift the buttocks and push the heels into the floor. Squeeze the buttocks while lifting it and the lower and middle back. The body's weight should be resting on the shoulders. Take three breaths and squeeze the buttocks and pelvic floor muscles. Slowly lower the buttocks and back, vertebra by vertebra, to the floor. Repeat three to four times initially, and build up to 10 repetitions. Things to remember when exercising At first, a person may only be able to perform an exercise three or four times. Build strength by practicing the exercises daily. Eventually, work up to 10 repetitions of each exercise per day. If a person stops doing the exercises, the muscles may weaken, and ED may return. Other types of exercise that can help Aerobic exercise can also benefit people with ED. People who practiced an aerobic exercise four times a week saw the best results, according to the authors of a 2018 systematic review. Each exercise session should be of moderate or high intensity and last a minimum of 40 minutes. Some examples of aerobic exercises include: cycling spin classes boxing rowing running skipping A person should keep up their aerobic exercise routine for at least 6 months. Exercise is essential for maintaining the health of the blood vessels and the heart. Also, people with cardiovascular disease have an increased risk of ED. Improving the diet Diet and weight loss are also important aspects of ED treatment and prevention. People with ED are more likely to be inactive and overweight. Alcohol also plays a role. Following dietary guidelines and limiting the intake of alcohol and foods with added salt, sugar, and fat will help to reduce the risk of developing ED. These efforts will also reduce a person's risk of stroke, metabolic disease, and cardiovascular disease, all of which are linked to ED. Takeaway A person with ED will often see improvement after making lifestyle changes. These should also reduce the need for medication and benefit overall health in the long term. Adjusting the diet and performing exercises, particularly those that target the pelvic floor muscles, can help to reduce or eliminate ED. |
|
#177
|
||||
|
||||
|
Re: Sexual Health News
Telling the difference between genital pimples and herpes
https://www.medicalnewstoday.com/articles/322679.php Genital herpes and genital pimples have similar characteristics, often appearing as small, pus-filled bumps on the skin. There are differences between genital herpes and pimples on the genitals, however, which can help a person identify each condition. The appearance of small pus-filled bumps on the genitals can cause worry. Although not all bumps are cause for concern, anyone who is in any doubt should consult their doctor. Pimples are the result of a buildup of dirt or oil that clogs up the pores. Genital pimples often appear pink or red and are filled with white pus. They are not a serious medical condition. According to the Centers for Disease Control and Prevention, genital herpes is a sexually transmitted infection (STI) that has no cure. Genital herpes can present as white or red bumps filled with a clear liquid or as red ulcers that are typically painful. According to the World Health Organization (WHO), approximately 417 million people worldwide have the virus that causes genital herpes. Symptoms of genital herpes vs. pimples Herpes and pimples share the following symptoms: both may appear as a cluster of red bumps both may itch both contain pus Herpes-specific symptoms  The herpes virus can lie dormant for years after exposure, and symptoms may appear any time. Sometimes people have no signs or do not recognize them. When an outbreak of genital herpes does occur, it usually presents as a patch of small red or white bumps or red ulcers. These lesions are often painful. Genital herpes may also appear on the buttocks or mouth in some cases. The pus-filled blisters will eventually burst, leaving an ulcer-like sore on the skin. People may experience additional pain when the blisters burst. It can take several weeks for a herpes outbreak to subside. The first outbreak, however, tends to be the most severe. People who have herpes may also experience additional symptoms. These symptoms may include: fever achiness headaches pain in the legs swollen lymph nodes vaginal discharge Lesions caused by genital herpes tend to feel softer than a pimple and can sometimes resemble a blister. Pimple-specific symptoms Genital pimples, by contrast, often feel firm to the touch. Pimples may appear one at a time or in small clusters. Pimples also tend to form near areas where sweat can collect. They may develop in areas where underwear or other tight clothing touches the skin, causing sweat and dirt to build up. Pimples develop within pores and will only rise above the skin surface if they accumulate enough pus. Pimples will leak thick pus or blood if squeezed or scratched. Genital pimples may itch, but unlike herpes lesions, they do not tend to be painful unless a person applies pressure to them. Pimples may also appear following intense exercise, heat, or humidity. Pimples will clear up quickly in most cases. What are the causes? Causes of genital pimples and genital herpes are entirely different. Causes of genital pimples Genital pimples are not contagious. They develop due to: clogged skin pores ingrown hair folliculitis Causes of genital herpes A virus known as herpes simplex virus (HSV) causes genital herpes. The virus can easily spread from person-to-person through sexual activity. There are two types of herpes virus. HSV-1 is generally referred to as oral herpes as it tends to form in or near the mouth. HSV-2 typically develops around the genitals and is the most common type of sexually transmitted infection. Sexual activity can spread both types of the herpes virus. Practicing safe sex can help prevent the virus from spreading. However, people can still contract the virus even when using a condom or dental dam. Risk factors A person is at high risk for developing genital pimples when: they are extremely sweaty wearing tight clothing that can trap sweat and debris under the skin shaving over pubic hair the weather is hotter and more humid People can contract genital herpes through sexual activity with anyone who has the virus.  People most at risk are sexually active people with multiple partners. It is still possible for herpes to spread from person-to-person even when using a condom or a dental dam and a person is not experiencing a flare. How are they diagnosed? Genital pimples tend to clear up quickly on their own. However, people should speak to their doctor if the pimples do not clear up with simple routine changes or if the bumps appear shortly after sexual activity. A doctor can diagnose genital herpes by carrying out a test to see whether the HSV virus is present. Potential tests include: HSV DNA test HSV culture herpes serologic test If a doctor confirms genital herpes, they may also check for additional STIs. Treatment Treatment options vary according to whether a person has pimples or herpes. Pimple treatment It is not usually necessary to treat genital pimples with anything more than good hygiene practices, such as cleaning the genital area more thoroughly or frequently. Other treatment options include: applying ointments that contain acne medication using antibacterial soap applying antibacterial creams using a warm compress and applying it a few times a day trying essential oil ointments with antibacterial properties Herpes treatment Herpes treatment, by contrast, usually requires medical intervention. A doctor will typically prescribe antiviral medications to combat the herpes infection. People should take the recommended doses and avoid sexual contact until the outbreak subsides. A doctor may recommend over-the-counter (OTC) pain medications or prescribe slightly stronger medicines if the lesions are painful. Can they be prevented? People can take steps to avoid developing either genital pimples or herpes. To prevent pimples, a person can try: washing their genitals at least once a day and after any activity that causes the person to sweat wearing loose-fitting clothing that does not cause friction bathing or showering regularly avoiding shaving pubic hair A person can help prevent genital herpes by: always using a condom or dental dam during sexual activity avoiding having sex with someone who has herpes avoiding having sex during a partner's flare Takeaway People may confuse genital herpes and genital pimples. Signs that the pus-filled bumps are herpes and not pimples include. pain associated with the bumps additional symptoms appearance of bumps following sexual contact with a partner Pimples should clear on their own and are often preventable. Herpes will cause a person to experience flares and will usually require additional medical treatment. |
|
#178
|
||||
|
||||
|
Re: Sexual Health News
How are HPV and herpes different?
https://www.medicalnewstoday.com/articles/322674.php HPV and herpes are both common sexually transmitted infections that can affect a person's skin. However, each virus involved is distinct. The infections require different treatments, and they can have different long-term effects on the body. HPV is an abbreviation for the human papillomavirus. The herpes simplex virus (HSV) causes herpes. There are also different types of each of these viruses. Each type causes different symptoms, and they can affect different parts of the body. There is no cure for either HPV or herpes. In this article, we look at the distinctions between HPV and herpes, including their symptoms and methods of treatment and prevention. The key differences between HPV and herpes We summarize the most important differences between these two viral infections in the table below: 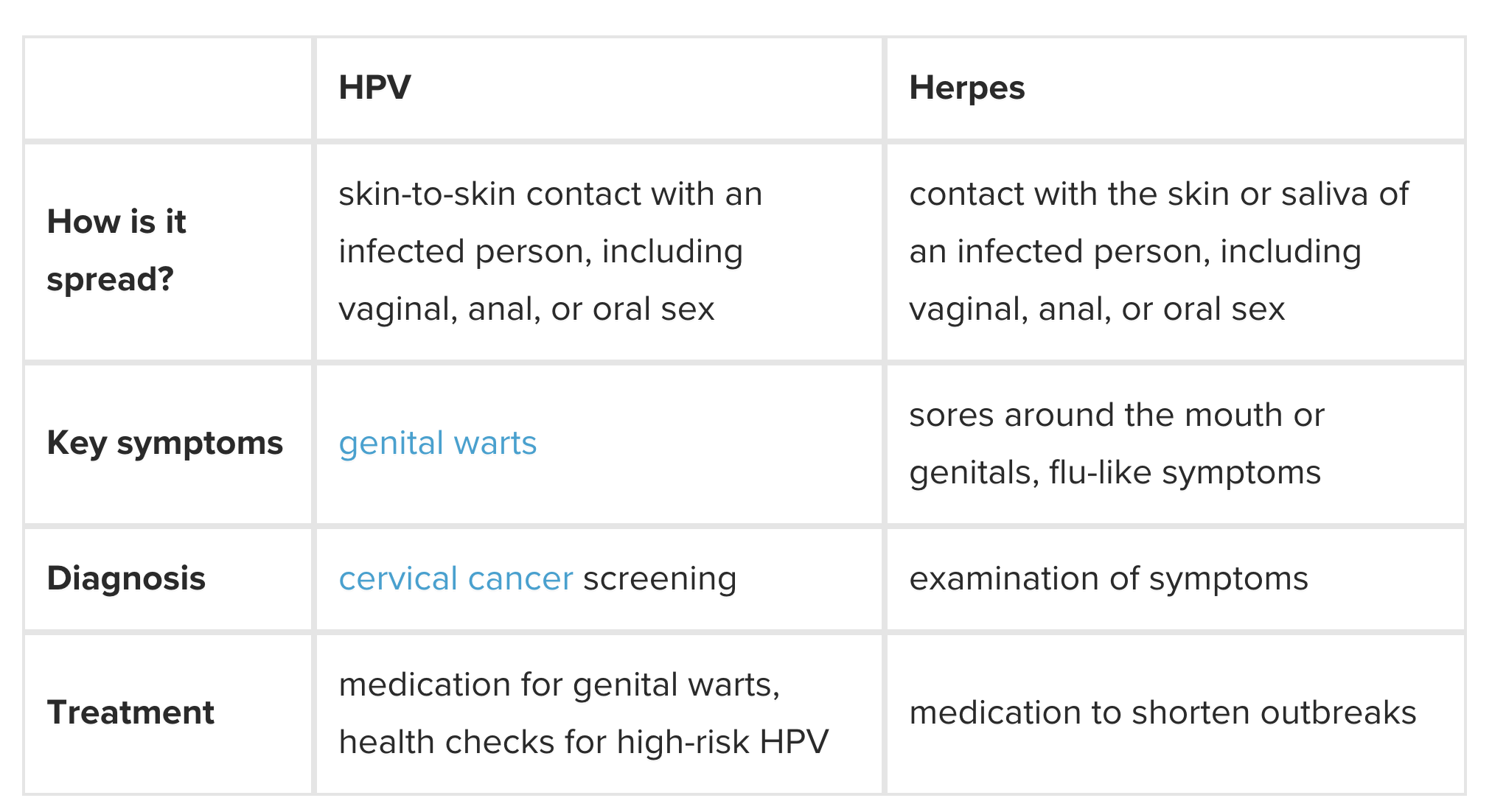 Herpes There are two different strains of the herpes virus: HSV-1 typically causes oral herpes, which affects the skin around the mouth. It can occasionally affect the skin around the genitals. HSV-2 typically causes genital herpes, which affects the skin around the genitals and anus. It can occasionally affect the skin around the mouth. In the United States, more than 1 in 6 people aged 14–49 years have genital herpes, while around 50 percent of adults in the country have oral herpes. A person can transmit either form of herpes during oral sex. Oral herpes can spread through kissing, and many people get it as children. Both types of herpes cause itchy blisters to form on the skin, and these can break to develop sores. When the blisters appear in or around the mouth, they are known as cold sores. Cold sores can also appear on the lips, and they may appear in clusters. The surrounding skin may be red, chapped, or irritated. The sores do not usually last longer than a few weeks. Herpes blisters can come and go. When they appear, this is often called an outbreak. The first time a person has an outbreak, they may also have symptoms of the flu. Outbreaks usually become less painful over time. As a person ages, the outbreaks tend to occur less frequently and last for shorter periods. Some people stop having them altogether. Herpes blisters are usually filled with fluid, and they can be painful. They appear grouped together on the skin, and they may appear around the: vulva vagina inside of the thighs anus penis Additional symptoms associated with genital herpes include: itching pain around the genitals a burning feeling when a person pees Herpes is usually not a life-threatening condition. HPV HPV is the most common sexually transmitted infection in the U.S., where 79 million people have it. There are many types, or strains, of HPV, and they can cause different symptoms. Most strains cause no severe health issues, but some can cause cancer. The medical community considers HPV types 6 and 11 to be low-risk strains because they are unlikely to lead to serious medical problems. They do, however, cause 90 percent of all genital warts. Genital warts can develop on the: penis scrotum anus vulva vagina cervix These warts look soft, pale, and fleshy. They do not cause symptoms, and medical professionals can remove them if necessary. High-risk strains of HPV can lead to cancer, and these strains are responsible for most cases of cervical cancer. Some types of HPV and also cause cancer of the genitals, anus, mouth, or throat. The Centers for Disease Control and Prevention (CDC) recommend that females aged 21–65 years attend screenings for cervical cancer, also known as a Pap smears or Pap tests. This screening can detect any changes HPV has made to the cells. Who is at risk? Anyone who is sexually active is at risk of contracting HPV unless they have received a vaccine for the virus. People are at risk of contracting herpes if they are sexually active or come into contact with the skin or saliva of others with the virus. Individuals with weakened or suppressed immune systems can have an increased risk of contracting herpes and HPV. A person is unlikely to contract HPV if their only sexual partner does not have the virus. It is important to remember that herpes and HPV do not always cause symptoms. Only testing can show whether a person has an infection. Diagnosis Testing for herpes is not usually part of a routine sexual health scan. If a person has symptoms, they can request a test from their doctor or a sexual health clinic. It is not possible to test for every type of HPV. Also, the infection is so common that an HPV test is not part of a routine sexual health screening. A cervical screening checks for high-risk forms of HPV that can cause cervical cancer. Some people with herpes or HPV have no symptoms or symptoms so mild that a person may not be aware of them. A medical professional will usually only be able to diagnose HPV or herpes if a person has symptoms. After checking the symptoms, they may offer testing if it is available. Treatment There is no cure for herpes or HPV. However, treatment can address the viruses' symptoms and complications. HPV treatment: if a healthcare professional detects precancerous changes after testing, a person will undergo further monitoring tests a medical professional can remove a person's warts, though they rarely cause symptoms and removal is not always necessary Herpes treatment: a person can take medication to shorten outbreaks reduce their frequency wearing loose clothing can help reduce irritation from blisters keeping skin clean and dry supports the healing of sores pain relief medication can help with symptoms A person may not require treatment if they have no symptoms or their symptoms are mild. Complications Certain strains of HPV can cause cancer, which often develops long after the initial infection. Some people with these strains of the virus do not develop cancer. Screening and awareness of early cancer symptoms can help to ensure timely treatment. During an outbreak of genital herpes, a person will have blisters on their skin, which can easily break. A person with broken skin on or near the genitals has a higher risk of contracting HIV from a partner because the broken skin makes it easier for the virus to enter the bloodstream. If a person with HIV is taking antiretroviral medication as prescribed and has a consistently suppressed viral load, medical experts believe that there is effectively no risk of sexually transmitting the virus to an HIV-negative partner. Research into this is ongoing. Complications during pregnancy A pregnant woman can safely attend a cervical screening for HPV. In some cases, an HPV infection can lead to pregnancy loss or delivery before the full term. Genital herpes can cause severe complications for pregnant women. Herpes can be passed to the baby during delivery. This can cause a serious infection called neonatal herpes. If a pregnant woman has genital herpes, a doctor may prescribe anti-herpes medication toward the end of the term. If there are symptoms of genital herpes close to the delivery time, a doctor will usually recommend a cesarean delivery. Prevention A person can greatly reduce the risk of transmitting HPV and herpes by using a condom or dental dam during every sexual encounter, including oral sex. However, these viruses can live on the skin around the genitals, so it is possible to get HPV or herpes even when using protection. Oral herpes spreads through contact with saliva or a cold sore. This can result from mouth-to-mouth contact, such as during kissing. The virus cannot live outside of the body, so a person cannot contract it from objects, such as bedding or toilet seats. A person with genital herpes can take steps to avoid passing it to a partner. These can include: taking anti-herpes medication every day avoiding sexual contact during outbreaks Avoid touching sores, as this can spread the virus to other parts of the body. There is no vaccination for herpes, but there is an HPV vaccination. The CDC recommend that children aged 11 and 12 years are vaccinated for HPV. The vaccine is also available for adults up to the age of 27, if they did not receive the vaccine as children. Takeaway HPV and herpes share similar qualities, but it is important to understand their differences. Herpes can cause more irritation and discomfort, but HPV often has a more serious impact on long-term health. There is no cure for herpes or HPV, but a person can take steps to prevent the symptoms and transmission of both. The HPV vaccination is the most effective method of preventing this virus. Using condoms and dental dams can reduce the risk of contracting sexually transmitted infections. Planned Parenthood have more information about how to practice safer sex. |
|
#179
|
||||
|
||||
|
Re: Sexual Health News
Self-lubricating latex could boost condom use: study
https://news.abs-cbn.com/life/10/17/...ndom-use-study PARIS, France - A perpetually unctuous, self-lubricating latex developed by a team of scientists in Boston could boost the use of condoms, they reported Wednesday in the journal Royal Society Open Science. Protective sheaths made with the specially treated membrane take on a slick and slippery quality in the presence of natural bodily fluids, lab experiments showed. And unlike water- or oil-based lubricants added to commercially available condoms, the hydrophilic -- or liquid-loving -- latex retains its "slippery sensation" almost indefinitely. "A majority of participants -- 73 percent -- expressed a preference for a condom containing the lubricious coating, agreeing that an inherently slippery condom that remains slippery for a long duration would increase their condom usage," the study concluded. "Such a coating shows potential to be an effective strategy for decreasing friction-associated pain" -- for women and men -- "and increasing user satisfaction." Condoms prevent pregnancies and the spread of sexually transmitted diseases. Some are made of lambskin but most are synthetic, manufactured from latex or polyurethane. Without lubricants, however, all of these materials will chaff during "repeated articulations," the term of art used by the researchers to describe thrusting motions. Added emollients wear off with use. Discomfort during intercourse and reduced pleasure -- noted by 77 percent of men and 40 percent of women in a nation-wide survey in the United States -- are often cited as reasons for not using condoms at all. Researchers at Boston University led by Mark Grinstaff addressed these problem by adding a thin polymer coating of moisture-activated molecules that entraps liquid rather than repelling it, as latex does. The polymer-treated condoms did not affect the latex, and "provides consistently low friction even when subjected to large volumes of water, or 1000 cycles of articulation," the study reported. In touch tests, volunteers expressed a strong preference for condoms that were "inherently slippery" and remained so for a long time. Because the material has yet to be approved by the US Food and Drug Administration (FDA), the liquid-loving latex has yet to be tested during intercourse. But more than 90 percent of the volunteers said they would consider using the coated condoms, and more than half said they would likely use condoms more frequently if the perpetually slippery ones were commercially available. |
|
#180
|
||||
|
||||
|
Re: Sexual Health News
Why has my penis gone numb?
https://www.medicalnewstoday.com/articles/322694.php When a person loses some or all of the feeling in their penis, it has become numb. The penis contains many nerve endings, and it is usually very sensitive. Numbness can occur when a person sits in a certain position for a long time. It can also result from low testosterone levels, another health issue, or an injury. People should see their doctor if their penis or testicles have become numb for no apparent reason. In this article, we look at what can cause numbness in the penis and how to regain sensitivity. Symptoms The penis has become numb when a person cannot feel sensations that they usually would, including feelings of touch or stimulation. Symptoms of numbness can vary from person to person. For some, it feels similar to an arm or leg falling asleep. Others may feel as though the circulation to the area has been cut off. Some people with numbness report feeling very little stimulation, while others feel nothing, even from heavy stimulation. Other symptoms can accompany numbness, depending on the underlying cause. These symptoms can include: a loss of sensation in the testicles, perineum, or the skin around the penis a burning or tingling, needle-like feeling coldness in the penis or testicles blue or purplish skin What causes a numb penis? A number of issues can lead to a loss of sensation, and some activities and lifestyle factors can increase the risk. The following can cause numbness in the penis: Injury An injury on or around the penis can cause it to become numb. This can result from damage to certain nerves or blood vessels. Usually, sensitivity will return in time. If it does not, speak to a doctor. The following can lead to pressure or injury to the penis or groin area: Riding a bicycle. The bumps and friction of the road can injure the perineum, testicles, and penis. Cycling can also place pressure on the groin and temporarily restrict nerves or blood vessels, leading to penile numbness. Sitting for too long. Sitting on uncomfortable or unpadded chairs for long periods can put enough pressure on the penis or perineum to result in injury. The perineum should not support the weight of the body. General irritation. Soaps and other hygiene products are more likely to irritate the sensitive skin on and around the penis. Using gentle, hypoallergenic soaps can help. Friction from tight clothes. Tight or rough underwear can irritate the penis, causing an itchy or tingling sensation. This kind of clothing can also cause redness, especially around the tip of the penis. Sex- or masturbation-related injury During sexual activity, the erect penis is not flexible. This rigidity can put the penis at risk for fracture or bruising, which can cause pain, irritation, numbness, and changes in color. Vigorous or excessive friction from masturbation and other types of sexual activity can also cause injury that leads to numbness. If a person notices a reduction in sensitivity, it may help to cut back or try different forms of masturbation. Damage can also result from using a pump, which sucks blood into the penis to achieve an erection. Numbness, bruising, cuts, and red or purple spots called petechiae may appear on the skin. Penis rings can help some people with erectile dysfunction, but overuse can lead to bruising and other types of damage. Low testosterone Testosterone is an important hormone with wide-ranging effects, including a role in regulating muscle mass and sex drive. After puberty, testosterone levels gradually decline, and many older adults have low levels. However, low testosterone can also affect younger people. When testosterone levels drop, a person may notice a reduction in pleasure from sexual activity. As a result, they may mistakenly believe that their penis is numb. Low testosterone can lead to numbness, but usually not when it comes to pain, so a person would still feel it if the penis or scrotum were pinched, for example. Other symptoms of low testosterone can include changes in mood, sex drive, and energy levels. Nerve problems Problems with the nerves in the area can cause numbness in the penis, testicles, and perineum. A number of health issues can affect the nerves and result in numbness. An individual may experience this numbness in the lower body and groin area. Some of these issues include: diabetes lupus multiple sclerosis (MS) cancer and its treatment vascular disease Peyronie's disease Peyronie's disease is a less common cause of penile numbness. A buildup of scar tissue, called plaque, within the penis characterizes this disease. The scar tissue can be less sensitive than regular penile tissue, and some people experience desensitization or numbness. Prostate cancer The prostate plays an important role in the reproductive system. It produces the fluid that carries sperm and helps to push out the fluid during ejaculation. Damage to the prostate, from a tumor, for example, can lead to numbness, tingling, and other changes in the penis. Also, a person may urinate more frequently than usual or have trouble urinating, among other symptoms. Treatment for a numb penis When numbness results from injury, it will usually heal with the injury. When an underlying condition is responsible for the numbness, treating or managing the health issue will usually resolve this symptom. The following methods can help to alleviate penile numbness: Changing lifestyle habits Because sitting in certain positions or on hard, uncomfortable furniture can cause numbness, a doctor may recommend: taking short breaks throughout the day standing whenever possible adjusting the sitting position changing chairs For cyclists, using a different bicycle seat can help to prevent pain and numbness around the groin after long-distance rides. Altering the angle of the seat can also cause it to absorb more of the shock and pressure from the road. Medications A doctor will usually prescribe medication to treat long-term medical conditions, such as diabetes, MS, and Peyronie's disease. Monitoring and controlling blood sugar levels can relieve symptoms in people with diabetes, who may need to take additional medication to prevent nerve damage. In advanced cases, diabetes can result in serious nerve damage known as diabetic neuropathy. People with Peyronie's disease can take medication that breaks down the scar tissue and collagen forming in the penis. This should control their symptoms. Raising testosterone levels A person with low testosterone may require hormonal treatment, which can come as pills, injections, or patches. Only take hormones with the guidance of a doctor. Outlook Numbness in the penis often results from an injury to the groin area. A person may sustain such an injury from vigorous sex, a long bike ride, or trauma. Treatment is usually relatively simple. Resting the penis can provide relief from common injury-induced numbness. If the numbness stems from a chronic condition or nerve disorders, the outlook may vary, but it is usually good. If symptoms persist after treatment, see a doctor. A person may have to try several techniques or treatments before finding one that works. Quote:
|
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |